Depression is more than just feeling sad or going through a rough patch. It’s a serious mental health condition that requires understanding, treatment, and a good recovery plan. With proper diagnosis and treatment, the vast majority of people with depression can overcome it and live productive, fulfilling lives.
The Scope of Depression
Depression is a widespread issue affecting millions of people worldwide. According to the World Health Organization (WHO):
- Depression is a leading cause of disability worldwide and is a major contributor to the overall global burden of disease.
- Globally, an estimated 280 million people in the world have depression (2021 data).
- At its worst, depression can lead to suicide. Over 700,000 people die due to suicide every year.
- Depression affects 5% of adults worldwide.
In the United States, the National Institute of Mental Health reports that an estimated 21.0 million adults had at least one major depressive episode in 2020. This number represented 8.4% of all U.S. adults.
Understanding Depression
Depression (major depressive disorder) is a common and serious medical illness that negatively affects how you feel, the way you think, and how you act. It’s characterized by persistently depressed mood or loss of interest in activities, causing significant impairment in daily life.
It’s important to understand that depression is not simply a case of “feeling blue” or a temporary reaction to life’s challenges. Some key points to understand about depression include:
- Neurochemical Imbalance: Depression is associated with imbalances in brain chemicals called neurotransmitters, particularly serotonin, norepinephrine, and dopamine. These imbalances can affect mood, motivation, and cognitive function.
- Brain Structure Changes: Studies have shown that certain areas of the brain, such as the hippocampus (involved in memory) and the prefrontal cortex (involved in decision-making and emotion regulation), may have structural differences in people with depression.
- Genetic Factors: While not a direct cause, genetic predisposition can increase vulnerability to depression. Studies suggest that depression is about 40% determined by genetics.
- Environmental Triggers: Stressful life events, trauma, loss, or chronic stress can trigger depressive episodes, especially in individuals with a genetic predisposition.
- Cognitive Patterns: Depression often involves negative thought patterns and cognitive distortions that can perpetuate and deepen the depressive state.
- Chronic Nature: For many, depression is not a one-time occurrence but a recurring condition that requires ongoing management.
It’s important to emphasize that depression is not a sign of weakness or a character flaw. People with depression cannot simply “snap out of it” — it’s a medical condition that requires professional help and understanding from those around them.
Signs and Symptoms of Depression
Depression can manifest in various ways, and symptoms can vary from person to person. For a clinical diagnosis of major depressive disorder, symptoms must be present for at least two weeks and represent a change from previous functioning. It’s important to note that not everyone who is depressed experiences every symptom, and the severity of symptoms can vary. Common signs and symptoms include:
- Persistent sad, anxious, or “empty” mood:
- This is often described as a feeling of hopelessness or pessimism that doesn’t go away.
- Many people describe it as a sense of emptiness or numbness, rather than sadness.
- This mood persists most of the day, nearly every day.
- Loss of interest or pleasure in hobbies and activities:
- Activities that were once enjoyable may no longer appeal to the person.
- This symptom, known as anhedonia, can extend to a loss of interest in social interactions, sex, or even favorite foods.
- Some people describe it as feeling like “the color has gone out of life.”
- Decreased energy, fatigue, feeling “slowed down”:
- Simple tasks may feel overwhelming and exhausting.
- This can manifest as taking longer to complete routine tasks or struggling to get out of bed in the morning.
- Some people describe it as feeling like they’re “moving through molasses.”
- Difficulty concentrating, remembering, making decisions:
- Depression can interfere with cognitive functions, making it hard to focus or make choices.
- This can affect work performance, academic achievement, and daily decision-making.
- Some people report “brain fog” or difficulty following conversations or plots in books or movies.
- Sleep disturbances:
- This can include insomnia (difficulty falling asleep or staying asleep), early-morning awakening, or oversleeping (hypersomnia).
- Sleep patterns may become erratic, with some people sleeping excessively during the day and being awake at night.
- Even when sleeping, the quality of sleep is often poor, leading to daytime fatigue.
- Appetite and/or weight changes:
- Some people may experience significant weight loss or gain (a change of more than 5% of body weight in a month).
- This can manifest as a complete loss of appetite or as comfort eating and cravings for specific foods, particularly carbohydrates.
- Thoughts of death or suicide, suicide attempts:
- These can range from a preoccupation with dying to actively planning suicide.
- Some people may express feeling that others would be “better off without them.”
- If you or someone you know is having thoughts of suicide, seek help immediately.
- Restlessness, irritability:
- Depression can manifest as agitation or inability to sit still.
- Some people may become more easily frustrated or angered than usual.
- This can strain relationships with family, friends, and colleagues.
- Physical symptoms that do not respond to treatment:
- These can include headaches, digestive disorders, and chronic pain.
- Some people experience backaches, chest pain, or joint pain that doesn’t have a clear physical cause.
- These symptoms often don’t respond to typical treatments, which can be a clue that depression might be the underlying cause.
- Feelings of worthlessness or inappropriate guilt:
- People may harshly criticize themselves for perceived faults and mistakes.
- They might feel guilty about things that aren’t their fault or that others would consider trivial.
- This can lead to social withdrawal as they feel unworthy of others’ company or support.
- Difficulty in relationships:
- Depression can strain personal relationships due to withdrawal, irritability, or lack of energy for social interactions.
- Some people may push away those closest to them, feeling that they’re a burden.
- Neglect of personal responsibilities and self-care:
- This might include failing to pay bills, neglecting hygiene, or letting household chores pile up.
- At work, it might manifest as missed deadlines or a decline in the quality of work.
It’s crucial to remember that depression can look different in different people. For example:
- In children and teenagers, depression might manifest as irritability, anger, or behavioral problems rather than sadness.
- In older adults, depression might be mistaken for dementia due to cognitive symptoms.
- In men, depression might manifest more as anger, irritability, or reckless behavior rather than sadness.
If you or someone you know is experiencing several of these symptoms for an extended period, it’s important to seek professional help. Early intervention can greatly improve outcomes and quality of life.
Types of Depression
Depression is not a one-size-fits-all condition. It can take various forms, each with its own characteristics and treatment considerations. Understanding these different types can help in recognizing symptoms and seeking appropriate help. Some of the most common types include:
- Major Depressive Disorder (MDD):
- This is the classic type of depression, characterized by persistent feelings of sadness, hopelessness, and worthlessness.
- Symptoms must be present for at least two weeks and represent a change from previous functioning.
- Episodes can be single or recurrent.
- Subtypes include:
- Melancholic features: Characterized by a loss of pleasure in almost all activities, worsening of symptoms in the morning, early morning awakening, and significant weight loss.
- Atypical features: Characterized by mood reactivity (mood brightens in response to positive events), increased appetite or weight gain, excessive sleep, leaden paralysis, and longstanding pattern of interpersonal rejection sensitivity.
- Persistent Depressive Disorder (Dysthymia):
- A chronic form of depression where symptoms last for at least two years in adults (one year in children and adolescents).
- Symptoms may not be as severe as in major depression but are long-lasting.
- People with this disorder may describe themselves as always having been “gloomy” or “joyless.”
- Bipolar Disorder:
- This condition involves alternating periods of depression and mania or hypomania.
- During depressive episodes, symptoms are similar to those of major depression.
- Manic episodes involve increased energy, reduced need for sleep, and sometimes reckless behavior.
- There are two main types:
- Bipolar I: Involves manic episodes that last at least 7 days or severe manic symptoms that require immediate hospital care. Depressive episodes typically last at least 2 weeks.
- Bipolar II: Involves a pattern of depressive episodes and hypomanic episodes, but not the full-blown manic episodes that are typical of Bipolar I Disorder.
- Seasonal Affective Disorder (SAD):
- Depression that’s related to changes in seasons, typically starting in the fall and continuing through winter months.
- Symptoms often resolve during spring and summer.
- It’s thought to be related to reduced sunlight exposure, which can disrupt circadian rhythms and lead to drops in serotonin levels.
- Treatment often includes light therapy along with other interventions.
- Postpartum Depression:
- This occurs in women after giving birth and is more severe than the “baby blues.”
- Symptoms can start anytime during the first year after giving birth but often begin within 1-3 weeks of delivery.
- It can interfere with the mother’s ability to care for her child and bond with the baby.
- In severe cases, it can include thoughts of harming the baby or oneself.
- Psychotic Depression:
- This is major depression accompanied by psychotic symptoms such as hallucinations or delusions.
- Psychotic symptoms are often related to depressive themes, such as delusions of guilt, poverty, or illness.
- This type of depression requires specialized treatment that addresses both the depression and the psychotic symptoms.
- Premenstrual Dysphoric Disorder (PMDD):
- A severe form of premenstrual syndrome that includes significant depression, irritability, and tension before menstruation.
- Symptoms typically resolve with the onset of menstruation.
- Situational Depression (Adjustment Disorder with Depressed Mood):
- This is a short-term form of depression that occurs in response to a specific stressful situation or event.
- Symptoms typically resolve once the individual has adapted to the situation.
- Atypical Depression:
- A subtype of major depression characterized by mood reactivity (mood brightens in response to positive events).
- Other features include increased appetite or weight gain, excessive sleep, leaden paralysis, and longstanding pattern of interpersonal rejection sensitivity.
- Treatment-Resistant Depression:
- This term is used when an individual hasn’t responded to at least two different antidepressant treatments.
- It may require a combination of treatments or alternative approaches.
It’s important to note that these categories are not always distinct, and individuals may experience symptoms that overlap multiple types. A mental health professional can provide a accurate diagnosis and recommend appropriate treatment based on the specific symptoms and circumstances.
Risk Factors for Depression
While depression can affect anyone, certain factors can increase the risk:
- Biochemistry:
- Differences in certain chemicals in the brain may contribute to symptoms of depression.
- Neurotransmitters like serotonin, norepinephrine, and dopamine play a crucial role in mood regulation.
- Hormonal imbalances, such as those occurring during pregnancy or thyroid problems, can also increase risk.
- Genetics:
- Depression can run in families, suggesting a genetic link.
- If one identical twin has depression, the other has a 70% chance of having the illness sometime in life.
- Specific genes, such as those involved in the serotonin system, have been implicated in increased susceptibility to depression.
- However, having a genetic predisposition doesn’t necessarily mean a person will develop depression.
- Personality Traits:
- People with certain personality traits appear to be more prone to depression:
- Low self-esteem
- Pessimism
- Being easily overwhelmed by stress
- Perfectionism
- Sensitivity to criticism
- These traits may interact with life events to increase vulnerability to depression.
- People with certain personality traits appear to be more prone to depression:
- Environmental Factors:
- Continuous exposure to violence, neglect, abuse, or poverty may make some people more vulnerable to depression.
- Chronic stress, whether from work, relationships, or other sources, can increase risk.
- Major life changes or traumas, such as job loss, divorce, or death of a loved one, can trigger depressive episodes.
- Chronic Illness or Pain:
- People with chronic medical conditions, such as diabetes, cancer, or heart disease, have a higher risk of depression.
- Chronic pain conditions are also associated with increased risk of depression.
- Medications:
- Certain medications can increase the risk of depression as a side effect.
- These may include some blood pressure medications, sleeping pills, and even some acne medications.
- Substance Abuse:
- Alcohol or drug abuse can both contribute to and result from depression.
- About 21% of adults with a substance use disorder also experienced a major depressive episode in 2018.
- Previous History of Depression:
- Having experienced a depressive episode in the past increases the likelihood of future episodes.
- Each episode may increase the risk of subsequent episodes.
- Age and Gender:
- Depression can occur at any age, but often first appears in the late teens to mid-20s.
- Women are about twice as likely as men to be diagnosed with depression, though this may partly reflect differences in help-seeking behavior.
- Hormonal Changes:
- Women may be at increased risk during hormonal changes such as perimenopause and menopause.
- Postpartum depression affects some women after childbirth.
- Seasonal Changes:
- Some people experience depression related to changes in seasons (Seasonal Affective Disorder).
- Social Isolation and Loneliness:
- Lack of social support and feelings of loneliness can contribute to depression.
- This has become particularly relevant during the COVID-19 pandemic.
- Childhood Trauma:
- Adverse childhood experiences, such as abuse, neglect, or loss of a parent, can increase the risk of depression later in life.
- Certain Medical Conditions:
- Some medical conditions are associated with an increased risk of depression, including:
- Thyroid problems
- Brain diseases such as Parkinson’s or multiple sclerosis
- Sleep disorders
- Nutritional deficiencies (e.g., vitamin D, B12)
- Some medical conditions are associated with an increased risk of depression, including:
- Socioeconomic Factors:
- Low income, unemployment, and financial stress can contribute to depression.
- A study in the Journal of Epidemiology and Community Health found that moving from the 25th to the 75th percentile of household income was associated with a 16% decrease in the odds of depression.
It’s important to note that having one or more risk factors doesn’t mean a person will definitely develop depression. Many people with multiple risk factors never develop depression, while others with no apparent risk factors do.
Diagnosis and Treatment
If you suspect you might be depressed, it’s important to consult with a healthcare professional. The diagnostic process typically involves:
- Physical exam: Your doctor may do a physical exam and ask questions about your health to determine if your depression may be linked to an underlying physical health condition.
- Lab tests: For example, your doctor may do a blood test called a complete blood count or test your thyroid to make sure it’s functioning properly.
- Psychiatric evaluation: Your mental health professional will ask about your symptoms, thoughts, feelings and behavior patterns. You may be asked to fill out a questionnaire to help answer these questions.
- DSM-5: Your mental health professional may use the criteria for depression listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association.
Once a diagnosis is made, treatment can begin. Treatment for depression often involves a combination of approaches:
- Medications:
- Antidepressants can help modify brain chemistry. Common types include:
- Selective Serotonin Reuptake Inhibitors (SSRIs)
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)
- Atypical antidepressants
- Tricyclic antidepressants
- Monoamine Oxidase Inhibitors (MAOIs)
- It’s important to work closely with a doctor to find the right medication and dosage.
- Antidepressants typically take 2-4 weeks to start showing effects.
- Side effects are common but often improve over time.
- Antidepressants can help modify brain chemistry. Common types include:
- Psychotherapy:
- Also known as talk therapy, this can help you learn skills to cope with negative feelings.
- Common types of therapy for depression include:
- Cognitive Behavioral Therapy (CBT): Helps identify and change negative thought patterns.
- Interpersonal Therapy (IPT): Focuses on improving relationships and social functioning.
- Psychodynamic Therapy: Explores how unconscious thoughts and past experiences affect current behavior.
- Therapy can be individual, group, or family-based, depending on needs.
- Combination of Medication and Therapy:
- For many people, a combination of medication and therapy is more effective than either treatment alone.
- A large study called the STAR*D trial found that about one-third of people achieve remission with their first antidepressant, and many more improve with a combination of medication and therapy.
- Electroconvulsive Therapy (ECT):
- This can be an effective treatment for severe depression that hasn’t responded to other treatments.
- It involves applying electrical currents to the brain to trigger a brief seizure.
- Modern ECT is much safer and more refined than its early implementations.
- It’s typically used for severe, treatment-resistant depression or when rapid improvement is necessary.
- Transcranial Magnetic Stimulation (TMS):
- This non-invasive procedure stimulates nerve cells in the brain with short magnetic pulses.
- It’s sometimes used when other approaches haven’t been effective.
- TMS is typically administered five times a week for 4-6 weeks.
- Light Therapy:
- Particularly useful for Seasonal Affective Disorder (SAD).
- Involves exposure to bright, artificial light to regulate the body’s internal clock.
- Lifestyle Changes:
- While not a substitute for professional treatment, certain lifestyle changes can support recovery:
- Regular exercise has been shown to have antidepressant effects
- Maintaining a regular sleep schedule
- Eating a healthy, balanced diet
- Reducing alcohol intake
- Practicing stress-reduction techniques like mindfulness or yoga
- While not a substitute for professional treatment, certain lifestyle changes can support recovery:
- Alternative Therapies:
- Some people find benefit from complementary therapies such as:
- Acupuncture
- Meditation
- Herbal supplements (e.g., St. John’s Wort, though this can interact with other medications)
- Always consult with a healthcare provider before starting any alternative treatments.
- Some people find benefit from complementary therapies such as:
- Ketamine and Esketamine:
- In recent years, ketamine and its derivative esketamine have shown promise for rapid treatment of severe, treatment-resistant depression.
- Esketamine nasal spray (Spravato) was approved by the FDA in 2019 for treatment-resistant depression.
- These treatments are typically administered under close medical supervision due to potential side effects.
The treatment is not one-size-fits-all. What works for one person may not work for another. It often takes time and patience to find the right treatment or combination of treatments.
Supporting Someone with Depression
If you know someone who is depressed, here are some ways you can help:
- Listen without judgment:
- Sometimes, people just need to express their feelings without receiving advice.
- Practice active listening: give them your full attention and reflect back what you hear to show understanding.
- Avoid minimizing their feelings or offering platitudes like “just cheer up” or “look on the bright side.”
- Encourage treatment:
- Suggest seeking help from a professional and offer to help make appointments or accompany them.
- If they’re reluctant, you might offer to help them research treatment options.
- Be patient – it can take time for someone to accept that they need help.
- Be patient:
- Recovery from depression can take time. Stay supportive and encourage small steps.
- Celebrate small victories and progress, no matter how minor they might seem.
- Remember that setbacks are common and don’t represent failure.
- Invite them to activities:
- Depression can be isolating. Continue to invite them to activities, even if they often decline.
- Suggest low-pressure activities like going for a walk or watching a movie together.
- Be understanding if they’re not up for socializing and don’t take it personally.
- Learn about depression:
- Understanding the condition can help you be more empathetic and supportive.
- Educate yourself about symptoms, treatments, and what to expect during recovery.
- This can also help you recognize warning signs if their condition worsens.
- Offer practical support:
- Depression can make everyday tasks feel overwhelming. Offer to help with:
- Household chores
- Grocery shopping
- Child care
- Driving them to appointments
- Depression can make everyday tasks feel overwhelming. Offer to help with:
- Be aware of suicide risk:
- Take any talk of suicide seriously.
- If you’re concerned about immediate suicide risk, don’t leave the person alone.
- Remove any potentially lethal items from their environment if possible.
- Call a crisis hotline or emergency services if necessary.
- Encourage healthy habits:
- Gently encourage them to:
- Stick to a regular sleep schedule
- Eat nutritious meals
- Get some form of exercise, even if it’s just a short walk
- Offer to join them in these activities if appropriate.
- Gently encourage them to:
- Avoid alcohol and drug use:
- Substance use can worsen depression and interfere with treatment.
- If you spend time together, suggest activities that don’t involve alcohol.
- Take care of yourself:
- Supporting someone with depression can be challenging. Make sure you’re also attending to your own mental health needs.
- Set boundaries to avoid burnout.
- Consider joining a support group for friends and family members of people with depression.
- Be consistent:
- Regular check-ins can make a big difference.
- Even a quick text or call to say you’re thinking of them can help combat feelings of isolation.
- Watch your language:
- Avoid phrases like “snap out of it” or “it’s all in your head.”
- Instead, use supportive language like “I’m here for you” or “You’re not alone in this.”
- Encourage social connections:
- Help them stay connected with others, but respect their boundaries.
- Offer to accompany them to social events if they feel anxious about going alone.
Remember, while your support is invaluable, you’re not responsible for “curing” your loved one’s depression. Encourage professional help and be a supportive presence in their journey to recovery.
When to Seek Emergency Help
While depression is treatable, it can become severe and, in some cases, life-threatening. It’s crucial to recognize when immediate intervention is necessary. Here are situations that warrant emergency help:
- Suicidal thoughts or behaviors:
- Any talk of suicide should be taken seriously.
- This includes statements like “I wish I were dead” or “Everyone would be better off without me.”
- Look out for behaviors like giving away prized possessions or saying goodbye to loved ones.
- Self-harm:
- This includes any intentional injury to oneself, such as cutting or burning.
- Even if the person says they don’t intend to seriously hurt themselves, self-harm is a sign that immediate help is needed.
- Psychotic symptoms:
- These may include hallucinations (seeing or hearing things that aren’t there) or delusions (fixed, false beliefs).
- Psychotic symptoms can occur in severe depression and require immediate medical attention.
- Inability to care for basic needs:
- If depression has become so severe that the person can’t eat, drink, or maintain basic hygiene, emergency care may be necessary.
- Rapid worsening of symptoms:
- If you notice a sudden and severe worsening of depressive symptoms, especially after a change in medication, seek immediate help.
- Severe anxiety or panic attacks:
- While not exclusive to depression, severe anxiety can often co-occur and may require emergency intervention if it becomes overwhelming.
If you think you may hurt yourself or attempt suicide, call your local emergency number immediately. In the United States, you can call 911 or the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255).
Also consider these options if you’re having suicidal thoughts:
- Call your mental health specialist.
- Call a suicide hotline number — in the U.S., call the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255).
- Seek help from your primary doctor or other health care provider.
- Reach out to a close friend or loved one.
- Contact a minister, spiritual leader or someone else in your faith community.
Remember, if you or someone you know is in immediate danger, don’t hesitate to call for emergency help. It’s always better to err on the side of caution.
Conclusion
Depression is a serious but treatable condition. With proper diagnosis and treatment, the vast majority of people with depression can overcome the disorder and live productive, fulfilling lives. If you’re experiencing symptoms of depression, don’t hesitate to seek help. Remember, reaching out for support is a sign of strength, not weakness.
The journey to recovery from depression is unique for each individual, but with persistence, support, and proper treatment, a brighter future is possible. Here are some key points to remember:
- Recovery is possible: Numerous studies have shown that with proper treatment, 70-80% of people with depression can achieve significant reduction in symptoms.
- Treatment is effective: A combination of medication and psychotherapy has been shown to be particularly effective, with success rates as high as 60-80%.
- Early intervention matters: The sooner treatment begins, the more effective it tends to be. Don’t wait to seek help if you’re experiencing symptoms.
- Persistence pays off: It may take time to find the right treatment or combination of treatments. Don’t get discouraged if the first approach doesn’t work – there are many options available.
- Self-care is crucial: While professional treatment is often necessary, self-care practices like regular exercise, healthy eating, and stress management can significantly support recovery.
- Support makes a difference: Having a strong support network can greatly improve outcomes. Don’t be afraid to lean on friends and family.
- Recurrence is preventable: With ongoing treatment and support, many people can prevent future episodes of depression.
- You are not alone: Millions of people around the world have experienced depression and found their way to recovery. Your experience is valid, and help is available.
Remember, depression is a medical condition, not a personal failing. Just as you wouldn’t hesitate to seek treatment for a physical ailment, don’t hesitate to seek help for depression. Your mental health is just as important as your physical health.
As you continue on this journey, be kind to yourself. Celebrate your progress, learn from setbacks, and always remember that seeking help is a sign of strength, not weakness.
And on the days when depression feels overwhelming, when the techniques don’t seem to be working as well as you’d like, remember this: You’ve survived every difficult day you’ve had so far. That’s a 100% success rate. You’re resilient, you’re capable, and you’re constantly growing.
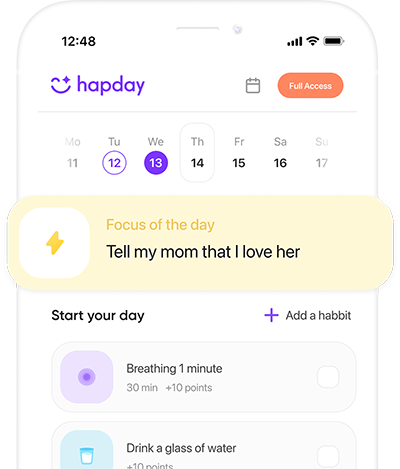
Build habits to support recovery with Hapday, Your Wellbeing Assistant
Join the millions of people using Hapday. Improve overall wellness & sleep.